Lisa Hulme-Moir
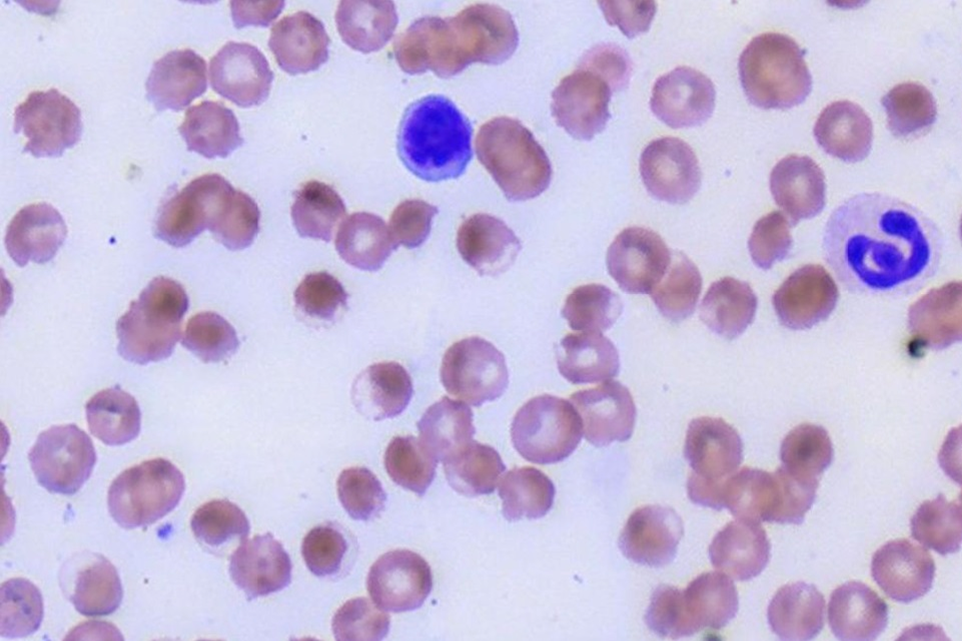
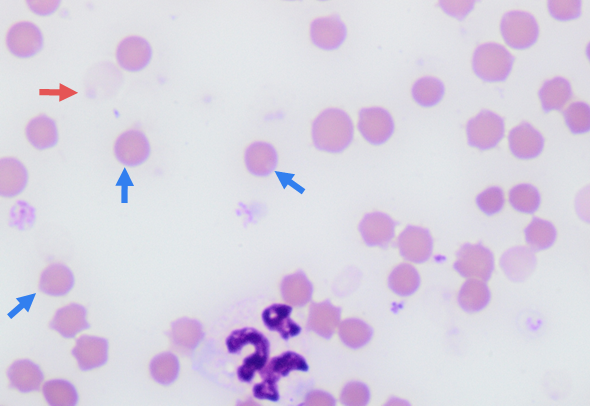
Figure 1 is a photomicrograph of a blood film from a four year-old male castrated Australian Kelpie. The dog had been in an induced coma with constant rate infusion (CRI) of propofol to manage hepatic encephalopathy due to acute liver failure. Haematocrit was 0.23 L/L.
What’s your diagnosis?
Answer:
Eccentrocytosis indicating oxidative injury and a likely haemolytic anaemia.
Discussion:
Multiple eccentrocytes are present in the blood film (Figures 1 & 2) indicating oxidative injury to the red cells. The anaemia was non/pre-regenerative at this point in time. Over the next two days the HCT fell to 0.14 L/L as the eccentrocytes were removed from the circulation. A strong regenerative response was evident five days later.
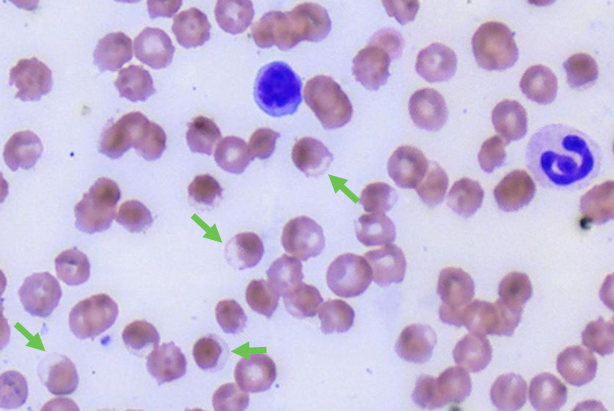
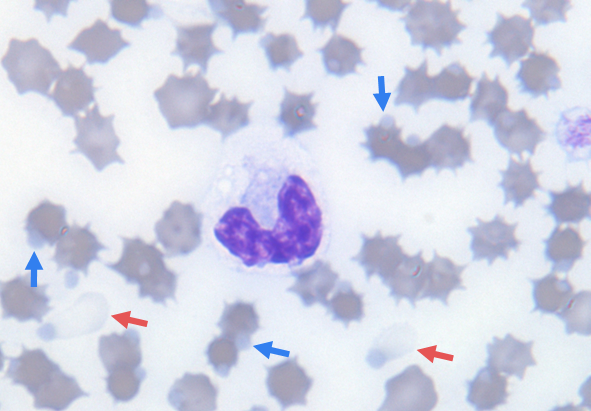
Prolonged or repeated exposure to propofol is a less frequently encountered cause of oxidative haemolytic anaemia in cats and dogs (Romans et al. 2020). In this case, oxidative stress due to the liver failure may also have been a contributory factor increasing the susceptibility of the red cells to oxidative injury. Interestingly, dogs have a tendency to develop eccentrocytes following oxidative injury whereas Heinz bodies are more typical in other animal species (Figure 3). Eccentrocytes are a result of direct oxidative injury to the red blood cell membrane and cytoskeleton. The opposing faces of the damaged cytoplasmic membrane stick to each other sequestering the cytoplasmic contents to one half of the cell. In contrast, Heinz bodies reflect denatured haemoglobin, which forms as a clump on the inner surface of the red cell membrane. In both cases, the presence of eccentrocytosis or Heinz bodies impairs the deformability of red cells causing them to become trapped and removed in the narrow vascular spaces of the spleen. As removal and destruction of the red cells is not immediate, many animals may be non or only mildly anaemic after initial exposure to an oxidant. A progressive anaemia, as seen in this case, may then develop over the subsequent 5-10 days. Clinical signs may therefore lag by some days after oxidant exposure. In some cases though, the integrity of red cell membrane may be impaired and intravascular haemolysis can occur causing more rapid clinical signs.
Aside from propofol, other causes of oxidative anaemia in dogs include onion or garlic (including foods that contain onion or onion powder such as baby food), zinc (e.g. swallowed objects or coins containing zinc), naphthalene (e.g. fumes from mothballs in cupboard/storage areas), paracetamol, vitamin K, and rodenticides. Eccentrocytes have also been reported in dogs with inflammatory disease, liver disease, diabetes and T cell lymphoma without exposure to an external oxidant (Caldin et al. 2005).
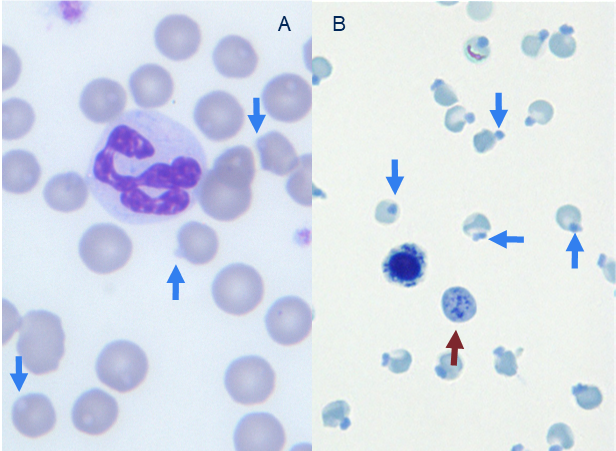
In cats, interpretation of Heinz bodies is a little more complicated. Feline haemoglobin contains more reactive sulfhydryl groups than other species making the haemoglobin more prone to denaturation. Additionally, the feline spleen has larger vascular spaces allowing red cells to pass through without deformation and making it less efficient at removing Heinz bodies (a process referred to as ‘pitting’). Consequently, it can be normal for up to 5% of feline red cells to contain Heinz bodies and increased Heinz body formation can be commonly noted in a range of diseases without anaemia or oxidant exposure (Figure 4). This includes hyperthyroidism, diabetes (particularly with ketoacidosis), liver disease and lymphoma.
In other animal species, Heinz bodies and eccentrocytes are always considered significant with the development of anaemia expected. Common causes of Heinz body haemolytic anaemia in cattle and sheep include brassicas, onions, zinc toxicity and copper toxicity (Figure 5). In the case of feed-related oxidants such as brassicas, anaemia may not develop until 1-2 weeks after ingesting the crop.
One final point about Heinz bodies aside from their pathological significance is their ability to interfere with tests on haematology analysers. This is particularly relevant to cats where Heinz bodies may occur more frequently. Red cells containing Heinz bodies are more resistant to the lytic agents used in some analysers and this can result in spuriously high leukocyte counts (Johnson et al. 2020). Heinz bodies also increase the turbidity of samples after lysis artifactually increasing the Haemoglobin concentration and it’s related indices, MCH and MCHC. Artifactually high reticulocyte counts may also be produced by analysers as red cells containing Heinz bodies have high autofluorescence which make them indistinguishable from reticulocytes stained with the fluorescent dyes used on these analysers (Camus et al. 2017).
References:
Caldin et al. A retrospective study of 60 cases of eccentrocytosis in the dog. Vet Clin Path, 34:224-231, 2005.
Camus et al. The fluorescent foible of Heinz bodies. Vet Clin Path, 46:9-10, 2017.
Johnson et al. Spurious marked leukocytosis in 2 cats with Heinz body haemolytic anaemia. Vet Clin Path, 49:232-239, 2020.
Romans et al. Oxidative red blood cell damage associated with propofol and intravenous lipid emulsion therapy in a dog treated for 5-fluorouracil toxicosis. J Vet Emerg Crit Care, 30:481-486, 2020.

