MICHAEL HARDCASTLE
We frequently receive incisional biopsies (e.g. wedge, Tru-cut or punch biopsies) of enlarged lymph nodes. Unfortunately these can be unsatisfactory for multiple reasons and excisional samples (i.e. removal of the entire node) are preferred.
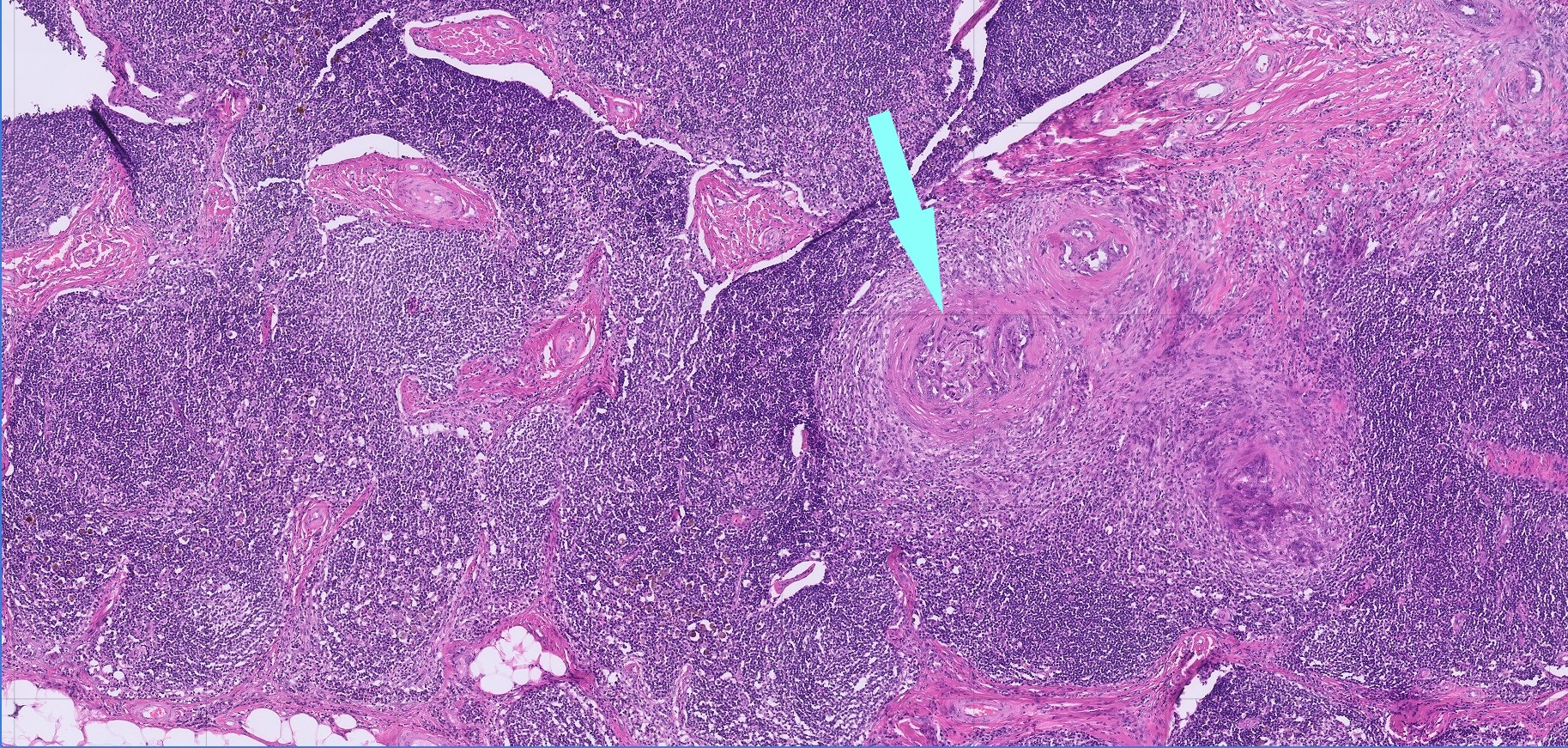
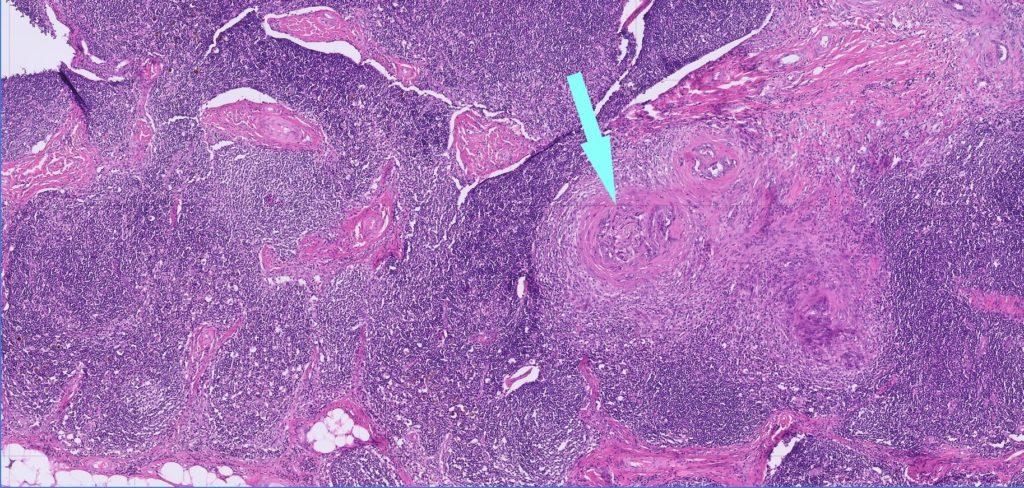
The main issues with incisional biopsies relate to sample distortion. Since lymphocytes are fragile and lymph nodes have a delicate supporting stroma, incisional biopsies (Tru-cut in particular) are often distorted by crushing or tearing artefact during the biopsy procedure and post-collection handling, leading to fragmentary sections with vague or unrecognisable cellular features (Figure 1). These artefacts make it very difficult to be sure whether the cells present are normal residents, neoplastic or inflammatory, or even what they are.
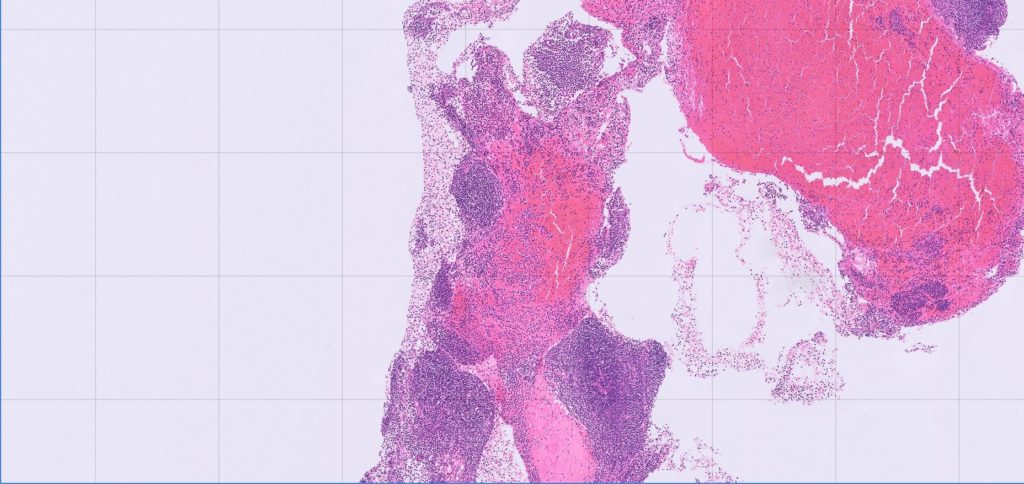
Furthermore, incisional biopsies may not be representative of the problem. Lymph nodes have a complicated architecture (see Figure 2) and the composition and volume of different areas of the node also changes with chronicity if they are hyperplastic or reactive nodes. This can make it difficult to rule lymphoma in or out if the biopsy is small or fragmentary, since it becomes difficult to know how representative it is.
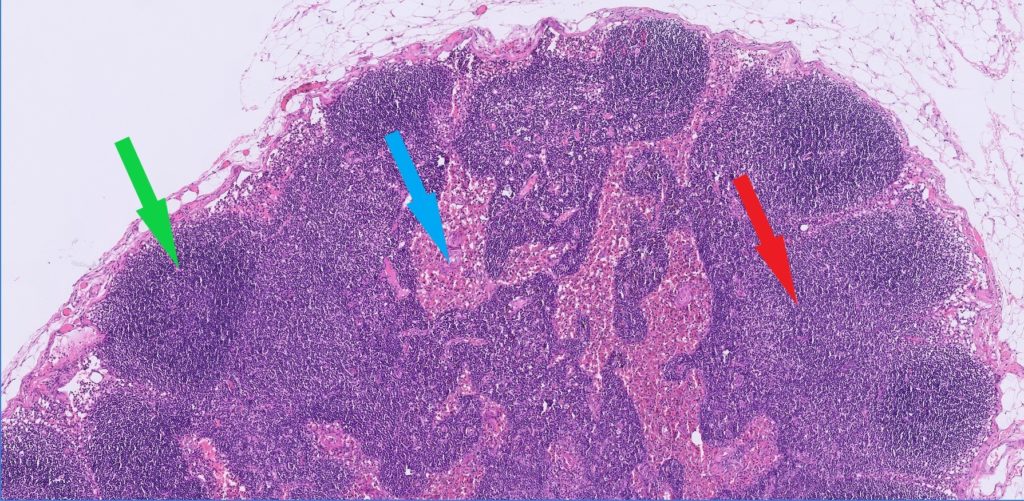
Some metastatic neoplasms (e.g. mast cell tumours or mammary carcinomas) may only occupy some areas of the node (Figure 3, arrow), and may be missed with small biopsies. We see samples in which reactive changes (especially necrosis) dominate the node and may be all that is represented in small samples. We also see samples of supposed lymph node that turn out to actually consist of salivary gland, adipose tissue or muscle; an excisional biopsy would help avoid mistaken identification of the node.
Finally, small biopsies can compromise follow up testing (e.g. special stains, immunohistochemistry, clonality) or recuts for second opinions/better sections with less artefact, since it is possible to exhaust the available tissue, and artefacts may affect the quality of follow up tests.